Perceptual difficulties/HPPD
In CPEP's 2023 survey of over 600 people who reported extended difficulties after taking psychedelic drugs, 26% report perceptual difficulties, the most common being visual distortions.
Individuals may experience phenomena similar to Hallucinogen Persistent Perception Disorder (HPPD), such as visual snow syndrome (seeing persistent flickering dots across the whole visual field), perceptual distortions, tracers (seeing lingering outlines of images or objects), and heightened sensitivity to light. These distortions can persistently disrupt daily activities, making it challenging to focus or engage with the environment. For some, these visual disturbances may manifest as a stretching or shifting of their surroundings:
“Multiple times throughout the day if I focus on something, my vision looks like it’s stretching and moving around gets worse the more I try to look for it.”
Visual hallucinations and disturbances typically persist for up to 6 months or between 12 and 24 months following a psychedelic experience. In about half of the cases, these issues are not severe and do not cause any disruptions. A quarter of those affected experience minor disruptions, while the remaining quarter report no disruptions at all.
Flashbacks and Traumatic Responses
Another aspect of perceptual difficulties after psychedelic experiences involves flashbacks or recurring trip-like episodes. These flashbacks can be distressing, resembling traumatic responses. Individuals may find themselves reliving aspects of their psychedelic journey unexpectedly, disrupting their sense of time and reality.
These flashbacks can be particularly challenging to manage, as they blur the line between past psychedelic experiences and present reality. For some, the trauma associated with these flashbacks can lead to significant emotional distress, impacting their overall well-being and quality of life.
Other Sensory and Perceptual Distortions
In addition to visual disturbances, individuals may also experience auditory distortions or hallucinations after psychedelic experiences. This can range from heightened sensitivity to noise to more extreme auditory hallucinations, including hearing voices or buzzing sounds. Other sensory distortions, including tactile, taste, and olfactory alterations, may also persist beyond the psychedelic experience. Additionally, some people experience extended distortions to their sense of time:
Time did not feel the same for up to a week afterwards, everything felt like it was moving a lot slower than it should’ve and this caused me to think I was going crazy leading to stress and low mood.
Coping Strategies
Coping with perceptual difficulties after psychedelic experiences requires an approach that addresses both the practical and emotional aspects of these challenges. Seeking support from mental health professionals who are knowledgeable about psychedelic experiences can provide valuable insights and coping strategies.
It is important to remember that perceptual difficulties after psychedelic experiences are a relatively common phenomenon and do not necessarily indicate long-term psychological harm. With time, patience, and appropriate support, many individuals find ways to integrate these experiences into their lives and move forward with a renewed sense of self-awareness and resilience.
Individuals experiencing visual distortions and hallucinations told us that educating themselves about their experience, cultivating an attitude of acceptance and surrender, meditation and prayer and spending time outdoors/in nature particularly helpful.
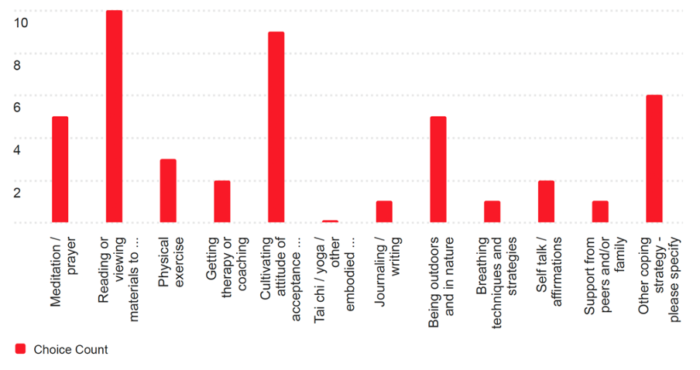
Here are some practices people generally have reported to find helpful to cope with challenging psychedelic experiences:
- Speaking to friends and family or attending a peer support group
- Speaking to a therapist, especially one who is familiar with psychedelic difficulties (CBT is often effective for anxiety and panic problems, although some also say they are helped by somatic therapy exercises that help regulate their nervous system).
- Cognitive practices like compassionate self-talk, cognitive distancing, and especially meditation and prayer
- Embodied self-care practices like exercise, yoga, walking in nature or body relaxation
- Finding useful information online and in books (e.g. the work of Stanislav Grof’s or “Breaking Open: Finding a Way Through Spiritual Emergency” by Jules Evans and Tim Read)
- Journaling
- Engage in creative activities like writing, art-making, or music
- Some people find medication helpful. Additionally, although controversial and risky, some may find that a subsequent altered state experience can help resolve their difficulties. However, this method carries obvious risks and should be approached with caution.
It is essential to explore and integrate these strategies in a way that resonates with personal preferences and needs, seeking support from professionals or trusted sources as needed.
Heather's story
Heather has suffered from depression for decades and has been on medication since she was 14. In 2021, she enrolled in a trial of psilocybin for depression in Canada run by a pharma company called Braxia. She says:
Right from the beginning, there were issues. First, they wanted me to taper off my medication on my own and I felt very uncomfortable about that, so I had to push to get a psychiatrist to help create a tapering plan. Even then, the process was very fast – under two months - given that I've been on medication for most of my life.
Heather went for her first psilocybin session in December 2021, at Braxia’s research clinic outside Toronto. She did not find it the most conducive setting for a psychedelic experience. The centre is in what she describes as a ‘rundown strip plaza in a suburb of Toronto, two doors down from Braxia’s ketamine clinic’. Inside the centre was ‘a narrow room, with no windows, no plants, and no natural light’. She also notes that, prior to her first dosing session, she was disturbed by the fact that the room was so cramped that the couch couldn’t fit flush against the wall.
She had a ‘meet and greet’ with the therapists for the trial before her session. This being the middle of the pandemic, they were wearing masks. She was also given a consent form which said this about the risk of extended difficulties:
1) Transient recurrence of disturbances in perception that are reminiscent of those experiences during one or more earlier hallucinogen intoxication. This side effect is seen rarely with recreational use of psilocybin, and has not been reported in scientific studies done under supportive clinical conditions.
2) Worsening of mental state after psilocybin experience (very rare and not seen in similar studies).
Heather ended up receiving three psilocybin doses over the six months of the trial. She had positive experiences during her first two sessions, and saw some improvements and some new challenges. She says:
I didn't feel suicidal anymore. My depression lessened, but life felt very hard, and I started to get very anxious over time. I think it was probably from being off antidepressants…I was destabilizing, and the team knew that.
She had a third experience in May 2022. ‘I didn’t sleep the night before. I was incredibly dysregulated. I went in sobbing. One of the team members was late. Right from the first intro session I felt they lacked the empathy and care of the other teams’
She went ahead anyway as she thought it was now or never and the session couldn’t be rescheduled.
Heather recalls:
I said to them, can you please help me regulate myself? And they gave a couple of suggestions, and then I said it again later on, and they're like, ‘we've already told you how to do this’. One of the guides, a psychiatrist said, ‘we're not here to guide you. We're just here to make sure you stay safe’. I went into the dosing session feeling unsupported and uneasy.
The first two session teams had discussed the issue of touch with her, and what would be helpful and acceptable to her. The third team didn’t mention it, so Heather brought it up.
They seemed very taken aback by the idea, then finally agreed. We determined that the gesture for me needing touch would be me putting out my hand. Then, at a certain point early in the experience, I put out my hand and no one was there to take it. I had to say, ‘Can someone please hold my hand?’ And it felt like they begrudgingly did it. Given my trauma history, that was incredibly traumatizing for me. In the previous sessions, I felt cared for. With this team, it felt like they didn't want to be there, and I had to take care of myself. This feeling was pervasive throughout the entire experience. Later on in the day, I was struggling to pull over a small table so I could eat my lunch, and no one offered to help me, unlike in previous sessions. Overall, it felt like a yucky experience.
In the days and weeks after that third session, she noticed her vision had altered.
The sky looked different. It was shimmering in a way that I couldn't really describe. I went for coffee with a friend, and she was wearing a black-and-white striped shirt. It was making me nauseous, like the stripes were moving. I also felt extreme anxiety, to the level of depersonalization, but I was still committed to psychedelics being the road to healing. At least I wasn’t depressed anymore. I was still committed to psychedelics as my route to healing.
Once the clinical trial had ended in June 2022, Heather still felt anxious and altered.
After that, things got much worse in terms of the level of distress I was experiencing. A week later, I still had some prescription ketamine that had been prescribed to me. I took it, hoping it would lessen my distress. That’s when the shit just hit the fan. My vision got so much worse in terms of colours, visual snow, blurred vision, and an inability to focus. I would go into these hyperarousal states, unable to regulate myself. I was taking benzos all of the time. I feel like something happened to my brain. I fried my nervous system, essentially, and have been struggling ever since then.
She’s definitely better than she was, but has been dealing with heightened anxiety, and now has formal diagnoses of PTSD, GAD and Hallucination-Persistent Perception Disorder (HPPD) – a disorder which supposedly never happens to participants in clinical trials or ‘safe settings’, and which one doctor told Heather ‘only happens to people who abuse drugs’. Since the trial, she has been unable to tolerate SSRIs or most other medications.
It's like I’ve been in the ocean using floaties for decades, and now all of a sudden the currents are really strong, I don’t know how to swim and I don’t have access to my floaties. It was devastating. I could barely function. I got a job in September 2022 but eventually went off on medical leave after six months.
She wrote to the Braxia team about the extended difficulties she was experiencing – severe vision issues, visual snow, blurred vision, intensified colours, difficulty focusing, difficulty tracking objects, episodes of cognitive dysfunction, severe anxiety / panic attacks, depersonalization and derealization. The clinical care lead expressed their sympathies and hoped she would get a referral for help, but it was hard – doctors either turned Heather down, cancelled appointments, or weren’t much help.
Thankfully, Heather did find some things that helped her: Guanfacine, neuro-rehab, vision therapy, supplements, meditation, and intensive psychotherapy. We asked Heather what symptoms have faded or responded to treatments and which remain an issue two years on.
She says the blurred vision has become less bad, and colours are now more or less back to normal. She also says the feelings of anxiety and derealization have lessened. However she still experiences some visual distortions and heightened sensitivity to light:
I’ve accepted that some experience of visual snow and floaters will likely be permanent features of how I perceive the world.
She adds: ‘I think it's important to note that I've spent thousands of dollars (if not tens of thousands of dollars) over the last two years to try to reclaim my health.’
In March 2024, Braxia published the results of the trial, showing a promising drop in depression and suicidality among the 18 participants who finished (nine of the 31 dropped out before the trial finished). It made no mention Heather's experience of HPPD. Braxia has since closed.
Further resources
For further information and support, the following web resources and support services are recommended:
- Perception Restoration Foundation: A charity to offer information and support to those experiencing HPPD.
- CPEP runs a free monthly online support group for people experiencing post-psychedelic difficulties on the last Sunday of every month.
- Here's an article by CPEP member Ed Prideaux about his own experience of HPPD
- This is a useful YouTube video about HPPD
- Psychedelic Clinic in Berlin: Clinic at Charité – Universitätsmedizin Berlin offering immediate support. Click here to get in touch.
- Psychedelic Support: Connect with a mental healthcare provider trained in psychedelic integration therapy and find community groups that can provide support.
- Fireside Project: The Psychedelic Support Line provides emotional support during and after psychedelic experiences.
- Institute of Psychedelic Therapy: The Institute for Psychedelic Therapy offers a register of integration therapists.