Severe anxiety after ayahuasca
This is an interview with Julie, who experienced several months of severe anxiety, weight loss, insomnia and existential confusion following an ayahuasca ceremony. She got in touch and we helped her find some resources that played a role in her recovery. Thank you for sharing your story Julie. Below is the transcript.
Jules
Okay, Julie, nice to see you. So, nice to see you. So thank you for agreeing to this interview, and I'm just going to ask you a few questions about your experience over the last 18 months, two years.
Julie
It's been just over a year. Thank the Lord. Yeah, so
Jules
you live in the US? Yep,
Julie
I live in Idaho.
Jules
Okay, are you an artist?
Julie
No, my husband is. That's Jeff. I'll drag him on in a bit.
Jules
So tell me a little bit about you know, the beginning of this story, then, where do you want to start?
Julie
So I'm a mental health counselor, and the last previous two years before Peru, I had become more and more intrigued with hallucinogens as interventions for all sorts of things, included trauma, anxiety, depression. In my family, I have a lot of history of addiction and and anxiety and depression, and I was blessed in that I never really struggled with it. Personally, I had a lot of challenges in my life at a really young age. I was like 18, I lost a son to crib death, so that was hugely traumatic. And then I grew up, my parents were both alcoholic, good people. They loved us, but they just, you know, they had their own struggles, and so didn't have the ideal experience. I grew up in a very Mormon community, which is also very tricky for lots of reasons, but I felt like I was really resilient. I went to school, was an occupational therapist for a while, and then, and then mental health, and I just was fascinated with research around hallucinogens and plant medicine and and I personally hadn't dabbled much in it. And part of that was growing up more when part of that was my parents being alcoholic. I really didn't even start drinking at all until I was in my 40s, you know, drinking wine and stuff. So I was a fairly, I would say, not abstinent, but when it came to that kind of thing, I just didn't have any experience. And so I just decided, from an experiential standpoint, I needed to understand it more before I dove in and and advocated or endorsed or, you know, and I did want to work in integration, and I happen to have a counselor who I brought on campus to talk about different interventions for mental health, and so I actually met with her the the month prior to going to Peru to start the integration process. So I felt prepared.
We looked into the to the retreat. I had a friend who went there 20 years before, and I previously, within the few months of going I tried mushrooms, and I had an experience just crying, sobbing, really, for three hours, and but it made sense to me, having lost my son, and that grief connected with that. And so it wasn't surprising, really, I did it in the way that they do the clinical intervention. So I had an eye mask on and just lay down and and cried. And so then I had an opportunity to DMA with my husband, and it was a beautiful experience, and it made complete sense to me how this could be used for couples counseling and all that. And so I didn't understand what Ayahuasca was, but there's a lot of you know stuff now out there about it, and I just decided to take the plunge. And we bought the tickets and and it was a beautiful it's a retreat area that's was built over 30 years ago. The guy who had built it was from the US, but it was one of the first of three, I think that was more, I think, geared towards people outside of Peru, you know, people who wanted the experience. And so he personally had a really positive experience with it, and just wanted to share it. And I think he, you know, I think I believe what he did was really good. The shaman that we met were beautiful people. They, I think, were really positive. He had died a few years. Uh, like around COVID, right before COVID. And so anyway, it was taken over
Jules
the original founder of the retreat center died, okay, yeah,
Julie
And so it's taken over by a much younger family member, and it was still, you know, very well suited for it, but really young and again, I think this is geared. They aren't schooled in Western culture and the needs of integration or the need to ease into it. We basically had the choice to drink the dosage that we wanted. And I felt like I again, I wasn't prepared. I didn't I remember listening to this interview, and it was from a comedian who wanted to stop drinking, and he was interviewing with Howard Stern, and he just said how freaky it was. But when it was over, it was over. And so in my mind, I'm like, well, when it's sober, it's over, no matter how scary it is, you know that? And I didn't have any anything counter to that. And so there were four ceremonies. First ceremony, I took a full cup, which was probably, I don't know, couple of ounces, couple of shot glasses. It was like a little and course, it was really intense. They call it the light show, just a lot of, I said it was like a like Vegas in a blender. You know, it's just like crazy, you know, some skeletons. And it wasn't, it really wasn't that creepy, though, and came out of it. And my husband and I, you know, went back, and, you know, our minds were blown for sure, but, but woke up, had the flower bath, and, you know, went back, had a integration. So it was every other night until the last two. And the last two are back to back. The third night, I did three or half a cup. So the first two full half cup, and then the fourth one, I went back up to three quarters a cup. And it just like I knew, as soon as I started throwing up, I knew it was in a bad place. And I, I, I asked for help, and they came over, and the shaman worked on me. My husband came over and held my hand, but at some point, I just had to roll over, and I just said I was alone and and it was just like bolts of energy or electricity just convulsing through my body, and I just laid there, and I just felt like I was at the mercy of of this energy. And anyway, that I don't know how long that lasted. Finally, you can, you know, it peaked, and it started to mellow out. A storm moved in and and the rest of it was quite beautiful with the storm, and we're in a maloca, and the rains coming through the screens, you know, just the midst of it and the thunder around us. And you know, I we got to the end of it, and I just assumed it was over, and we went back and had the flower bath, and my husband and I were scheduled to fly out that very next day, so we got went a ride back into town, and I had my first panic attack when I was on the plane. And that's a long plane ride, you know, and so that was, and luckily, had been a drill. That was the only thing that that I could use. And then we made it to the airport, the Salt Lake airport, finally, and then, or the LA Airport, had to sleep a night on the floor. Made it home, I would say, for the the next month, I was in shock, although I instantly started losing weight, and that was super scary. I ended up, you know, at the lowest part of my weight, I was down 204 so then it just started becoming obvious that something was wrong. So,
Jules
Was it a very frightening experience? Was the experience itself kind of overwhelming? Do you think or possibly traumatic, just this feeling, yes, being at the mercy of this kind of energy? Yes,
Julie
Absolutely, it was traumatic and very overwhelming. I felt hostage. I felt hostage for those few hours and and my I was, you know, like I said, I was in shock, but when I asked for help, I just yeah, just the fear, because I knew that, that I had slipped over to a different Yeah. It was yeah, some something my system wasn't ready to handle, and and then I like, I said, I just felt like I had to surrender to it. And so I felt competitive, I felt hostage. And I would say, yes, that was traumatic,
Jules
yeah, because you felt control and at the mercy of it. And it was somatically, physically, was it painful as well? Just this feeling of, kind of, you described it as, like, bolts of energy? Yes,
Julie
it was physically, very uncomfortable. I felt, I don't know, a lot of it's just like my nervous system was so hyped up that being in my body just felt it, just I felt like it. It wasn't like I didn't. I, I don't know there was, it was a certain kind of death, and my body suddenly was no longer safe. And I think that that's what it felt like. My body did not feel like a safe place. Yeah, yeah.
Jules
Okay, so the experience itself was, was traumatizing, and then it's the leaving immediately as well, and having to, you know that? I mean, it's having to do a long journey. I mean, a similar thing happened to me at an Ayahuasca Retreat. The Retreat itself was kind of okay, but the day after, suddenly you're back in Iquitos, which is a shock, and then you are dealing with airports which are weird and flights which are weird things anyway, and quite dissociate little bit. Yes. Do you think that I mean that maybe didn't made it help, didn't help. Yes,
Julie
yeah, definitely didn't help. Yeah, just the over stimulation of an airport and being in the middle seat and not feeling like I just again, it was that same feeling of feeling hostage right in the plane, in that middle seat, and I'm just my my nervous system is just so jacked up and so, yeah, that didn't help at all.
Jules Evans
So you get back and you said you started losing weight. You were eating, eating. Normally,
Julie
I had no appetite, and I just, you know, the retreat, we were on a clean diet and very vegetable based, and so I lost a few pounds being there, but I came back, and I just had such a hard time eating. And so I went from what was closer to 120 in a matter of, I think, a couple of weeks, down 204 you know, two to three weeks. And so, you know, my husband especially concerned, and I was just trying to get through the days, and I I had to come back to a job. And so again, I was moving back into my life fairly quickly, and I was in shock, but suddenly, you know, my body is like I said. I it, I I didn't first start drinking coffee again, because I was already so anxious, and I just stuck with, you know, just fairly clean, but I had to start drinking shakes just to stabilize my weight, and kind of had to change my patterns of eating so I didn't continue to lose weight, and so I wasn't even enjoying eating. Eating became a chore, and that that was really hard, you know, because that's one of the pleasures of life, is being able to eat that felt like another loss.
Jules Evans
What other kind of symptoms were you experiencing?
Julie
The primary thing was the anxiety initially and and like I said, I my anxiety. I would have anxiety attacks. I had really significant anxiety when I woke up in the morning or at the sleep my. Sleep was really messed up and I going to sleep was super scary. I just would wake up and my husband, you know, would hold me or rock me, you know, just my shoulder. And I had started, I had taken, had a small script of Ativan, and so I started taking that just to help me calm down, like the panic attacks. But then very quickly, and I never took a lot of it, but psychologically, I became like, I just couldn't stop taking it, and that really bothered me. That was the hard part of this year, is just getting to a place where I didn't have to take it anymore so, and by the end, so I came back middle of September, by the end of October, I just felt like I needed to see a psychiatrist so my sleep, my weight, I I was crying almost every day in the morning, and just like i said i I felt like I did. I wasn't myself. I felt like I had just lost a part of myself. And, shame, regret, you know, just a lot of it, but I started counseling right when I got back to so she She really tried to help me make meaning of what was happening. But, yeah, it was a lot of tears, a lot of anxiety, and then eventually depression that that settled in, yeah,
Jules
so in terms of, was there, was it, was there particular concerns or fears, anxious thoughts or beliefs in your mind, or was it more Just a kind of physical feeling of unease?
Julie
No, it there. I felt like I just started having these intrusive thoughts that were connected to the anxiety and and that was really scary too, you know, just, I think as a kid, when I was dealing with the alcohol and growing up in a Mormon community that, you know, I was exposed to my parents dysfunction and the fear of going to hell, you know, and so part of that growing up, and you know, the the thoughts that come into your head, you know that are super scary, and as a kid, you can't control them, and I felt like I suddenly was had activated that part of my self That, again, is just, it's just based on fear and anxiety and so that, yeah, yeah. And of course, here's the other thing, not only my counselor, but I teach meditation. I teach yoga. I was still, I came back and was teaching an eight week course on campus. And as I was teaching it, I could be in a good place, but to practice it myself, from myself, was really hard, and so there was a lot of shame around that, too. And I had an eight week class that I'd set up to practice Mindful self compassion, to do an eight week class on my property, and I had to cancel it because I just knew I was incapacitated, that I was too compromised to do what
Jules Evans
I mean, right? So you a lot of resources, mental health, experience, meditation, experience, a lot of personal resilience. You've been through a lot in your life, but in that hurricane, these these tools, weren't that kind of in the acute crisis, they they weren't they weren't really much help at that time,
Julie
I couldn't access them for myself. And it was interesting because I read this article from this Carrie. I can't think of her last name right now, and when I would get these bits of reassuring, you know, information, it was so elevating. But she talked about being a counselor, and how she had this experience and that she needed somebody else's nervous system help, stable. Her and the struggle she had, and I actually reached out to her and set up a one on one, and, you know, and it was like, I think, 250 bucks or something. And my primary thing, I didn't want her for a counselor. I had a counselor already. I wanted her to normalize my experience, right? And she had written about it so beautifully, and when I got on with her, she absolutely refused to talk about her personal experience, even though she had written about it, and she just kept deferring back to me and that, you know, and again, was almost shaming, you know that I was taking medication and and she was really her energy, I don't know it was it that was really, that was disheartening, right? Yeah,
Jules Evans
this lady was a psychedelic integration therapist, yes,
Julie
yes, yes. And she also, she also writes a lot on behalf of the topic, you know, and you know, she's very much about promoting it. And so I think anyone that has a story that challenges it, I think her goal is to almost talk you out of it, like, you know, this is just what you need to do. And I've, I've had that a couple of times, where I've got on with healers, but they've never had the experience. You know, they work with ayahuasca and they work with integration, but they personally never had the experience,
Jules Evans
the experience of difficulties. Yes,
Julie
yes, and and so again, the message i i went to another guy by the name of Michael, and he same thing. He, he himself was in recovery, and his whole thing was, I needed to get straight with my with my God, and that I was getting in my own way and and again, it was just very patronizing and shaming and that this was my doing, you know. I told him I felt like, you know, I died. And he's like, Well, that's great, you know? Well, I wasn't ready for saying that. That's great, right? And so, man, you have to be so careful who you know you reach out to. And I would say that that the thing that was most helpful was when my husband came across your information and he emailed you, and surprisingly, you emailed back, like we just didn't expect that. And then there, you know, you really have helped walk us through so much of this, but it's like the people like Deborah Martin who have been through it, and they're so willing and have been so supportive of helping guide us through this, because they genuinely know the suffering and the isolation. So the isolation was the other piece for me. My world got so small because I couldn't tolerate social stuff, and so I had to withdraw. And here we're going into, you know, an Idaho winter, and the one thing I could keep doing was, you know, we're very active. And so, you know, I kept running and cross country skiing and snowshoeing, and that was the one thing I'd already established a really strong practice with. And so just being in my body, doing physical things was helpful, because
Jules
at what point was it a few months after the experience, or six months or
Julie 24:13
we contacted you? Yeah,
Jules Evans 24:16
gosh, maybe it was about six months after or something. I
Julie
uh, I think it was in the early part of the year, so, so mid September, so by January, I think we had connected with you, yeah, maybe February, yeah.
Jules
And what struck me those initial emails was you, you were trying everything. I mean, you were being very proactive. But of course, just, I could tell a bit that also your nervous system was just really out of kilter. So it was, you know, and you were, you were completely understandably, like, frightened, like a. I suppose maybe was one of the fears, like, what do I do? Is this? Is this? How do I get out of this state? Like, is this perfect? Yeah, yes. Am I going out with this, or am I going to get out of this? Yes,
Julie
and that was the scariest part. It's the not knowing. And, you know, I, I went to multiple providers here. I, you know, I started off with a psychiatrist in October, and it was just, I mean, bless his heart, you know, he was doing his job, but it was just too much medication, like Seroquel at night, and, you know, something to for blood pressure in the morning, to deal with the anxiety in the morning. And I'm still on Ativan. And very quickly it was just like, I can't, I can't do this anymore, and so I, I just kind of kept and thank goodness I had my integration therapist. She was the consistent provider that just really helped and supported me. I tried hypnosis, I tried acupuncture, I, you know, again, I I felt like in the beginning my body, because I did try SSRI in the beginning, but I felt like my system can tolerate it. And I think part of that was they tend to, I must have a sensitive system. And so the typical dosage that they would prescribe, I think was just too much, and I think my system was still jacked up. And so I I was so afraid that I had serotonin syndrome where I could no longer take anything with serotonin. And that really scared me. And so again, it's the you just want it fixed right away, and you don't understand, and again, I understand the neuroscience around, you know, neuroplasticity and how what we practice grows stronger. But I started from such a scary place, and and it was such a roller coaster. And there were days the other thing that I think I did right was I kept going to work, and that was hard. I mean, I would be crying. Jeff would drive me sometimes to work and I'm crying. I would have to shut my door sometimes and just start crying. And I had to step away from opportunities, like I was in a leadership thing, and my boss was amazing, and, you know, she just supported me having to step away from certain things, events and that kind of stuff, because my social anxiety had gotten so bad.
Jules Evans
Why do you think it was important to stay working
Julie
because I had to have some normalcy, or, like I had, I had to have a structure. And I think you, you had mentioned, and it's interesting, because I am a counselor, but I never, personally used the act, you know, yeah, approach, so, acceptance, commitment, therapy, and I remember, and you suggested that, and I asked you, I said, So are you saying I just need to accept this? And you said, No, but you accept the moment, and then you make choices based on your values, and that's what you commit to, right? And that's really the other thing. I just had to keep going cross country skiing. I had to keep showing up for work and helping people I had because my world had gotten so small, I had to gain these parts of my life viable so that I just didn't end up in this little, tiny, tiny place and I can see where people do because it's just the fear just keeps you retreating and retreating, right? So, yeah,
Jules Evans
it almost the fear can can be like a bully taking more of your energy, more and more of your attention, if you let it. Yes.
Julie
Yes, absolutely, yeah. So
Jules
it affected your work, but you kept going to it. It affected your social life. You said, you said, you got some social anxiety, and you stopped going to some kind of social occasions. It was affecting your sleep, which is hard, because it reduces your resources, your anxiety and and you're like, what's going on? None of this, I presume you had any idea could happen.
Julie
No, not at all. I was so ill prepared again. I just kept thinking, when it's over, it's over,
Jules Evans
and the retreat center. Did they? Did they give you any information that it can sometimes be an extended process, or like you know, that,
Julie
you know, I guess you know they talked about, you know, continuing to have to do the work after, but nothing like this. And, of course, we. Had to sign a lot of documentation, but it's supposed to be used as a screen, and it talks about, have you ever had trauma? Well, you know, I did, and I talked about that, and I understand now that trauma can be an indicator for someone who ends up with, you know, these extended, really uncomfortable outcomes. And so I feel like they have the screening forms and, you know, but there's no one on the other side that really is interpreting this information in way that they need to say, look, right?
Jules Evans
Are you prepared? I mean, so many people who look to these medicines at the moment or these substances have trauma. So that's, that's so I'm, we're going to get on to the things that helped and but you mentioned earlier, before we started recording, that you think this was one of the hardest things you've ever been through. I mean, just to give people a sense of, you know, what it's like to go through this, it's extremely hard, right? So,
Julie
and they have to put this in context. I mean, I, I've lost a child. However we are, are in life, we have the capacity to deal with great loss, right? We're actually wired for that and and it's relatable. So when you have a loss like that, you have people around you. You have people who can relate to you. Have people who've had their children that they've lost, right? So so you have this relatability that allows you not to feel so alone. The problem with this is that you come back home, nobody can relate to it, and so there's so much isolation in it, and then there's you chose to do it. So there's the shame and feeling you know just so stupid and ignorant that you'd you know, and even though I had my reasons for wanting to do it, and I still feel justified in that I didn't understand what I was saying yes to and that was very unwise on my part. But it's the isolation and then your body going through this, or an anxiety and grief is, again, I've had lots of grief in my life. I've never had to deal with this kind of anxiety, and it's paralyzing. And, you know, it's just and and again, not knowing there's no normal thing that says, Okay, this is going to last six months. Or, you know, it's, it's like an extended labor. Like, you know, what makes labor so hard when you're delivering a child is that you don't know when it's going to end. Especially now, you know back that when I had babies, you didn't have, you know, final blocks or whatever. So it's like months and months of that, like this horrible pain and discomfort, but you there's no even guarantee that it will end, yeah, and
Jules
very little information. And then when you do go to experts, sometimes they are shaming in some ways, or,
Julie
yeah, yeah, yeah, and I yeah, it just there's, there's so many unknowns to it, and I just the minute to minute life. I would say time slows down a lot now that it's been over a year. It was a year in September. Is that weird? That year feels like a weird period of time, and I, and I looking back, I you know, but when you're in it, it's like moving through mod, you just, but it's like you're in mud and you're trying to run because you're so scared and you can't, Wow,
Jules Evans
can I ask Jeff what it was like for you to go through this with you?
Jeff
Okay, how's it going? It's really good to see you, man. Nice to see you. So much. Thank you so much for all your help. I
Jules
mean, no, I was very moved by both of you reaching out. And I could feel how how hard it was, and how hard for you as well, Jeff, to see your loved one suddenly going through this, and for you both to go through
Jeff
It was the hardest thing, probably the hardest thing I've ever been through. Because initially I didn't know if she was going to live. I really thought when she was losing weight, that she was just going to waste away and die. Because it was just such a such an incredible impact on her that. Yeah, and it was just horrid. And, yeah, like we were saying, like you said a little while ago, there's just, there's no information about it. Very little. I just, you know, scoured to try to find things, and I found a few little things, but, you know, it was really hard, and not knowing when it would end, or if it would win, and, you know, if she would fully recover, that was, it was terrifying for me too, and I'm just so grateful this just so grateful. I mean, it's
Julie
Yeah, so grateful for you. Oh,
Jeff
you and, and just the fact that she's she's back, she's completely back to normal.
Julie
Well, mostly
Jeff
I'd say you're back. I mean things,
Jules Evans
these things change who you were, but you can still function. You can enjoy bright parts of life
Jeff
and, and you're vulnerable for sure, to some degree, but you're also eventually she'll be more resilient. I mean, I've been through some stuff with hallucinogens myself, some really bad experiences, and so I had, I had kind of a, I think, a better understanding than most people about what it must be like for her, but just, you know, being with her hour by hour. I mean, there were so many days when it was just minute by minute, she was just on the edge, and I just didn't know, you know, she would just start crying. And I just didn't know, you know, if this was the time, you know, she just like, wouldn't, wouldn't bounce back. You know, I was, I was really worried.
Julie
And, you know, I never like, I never wanted to kill myself, but I remember thinking like, I can't, I don't want to live like this.
Jules Evans
Yeah,
Jeff
it was, it was hard. It was really hard. And, you know, she would have little moments where she would be encouraged by something, and that would help. But, you know, the mind, the way the mind works when you're in a state like that, is it always goes to the most negative possibility, because you're in so much fear. You know, you want some kind of guarantee that it's going to be okay, but there is no guarantee. And so you always look for some way that it's not going to happen. You know, your mind does, and, yeah, it was a, it was a horrible struggle. And I know she was, at times, she was just, you know, so on the edge, you know, I would just rock her, just to try to calm her system down. But, I mean, she just, it was horrid. She couldn't sleep, and she couldn't be awake. It was just the most terrible place. And I'm so grateful that she's, she's healed, yeah, you know for the most part, oh, it's, it's been, it's been hard, but so wonderful now that we're out of it. So grateful.
Jules
Thank you, Julie. What would advice would you give to loved ones, if people, if, if, if, if they have partners or friends going through something like this, what is helpful to in terms of how to support them? What, because I spoke, becomes hypersensitive to to what people say as well, right? Oh,
Julie
so bad. Yeah, he, and he became very good at like because other people, even, you know, would say things and, you know, you just can't tolerate, you know, anything that's half like his. He would give me back. You know, body rubs all the time, and like I said, he would just gently rock me. He was always so encouraging that it was going to be okay. And you know that we were getting through this and and we had his willingness to look for information and anything that was relatable, like it's because of him that we found you. And you know, just making me food, he really helped me stabilize my weight, and just just so much love. I mean, he was and I know he was suffering, but he just, he just gave me this feeling that he really believed I was going to be okay, and I really needed that, yeah, for
Jeff 3
things too, because she's so sensitive to anything, yeah, so I try to just keep things, you know, if I knew that it was something was going to be triggered, or I would, and I would try to read things for beforehand, yeah, just to keep her from that stuff. Because, you know, I wasn't trying to be deceitful, but I just knew what it would do to her, and I knew that she didn't need that. She just needed every bit of positivity that she could, you know, that we could get. Yeah,
Julie
that's the tricky part, too, about other people's. Stories, because they can also be triggering in a in a very Yeah, yeah,
Jeff
right. I could get a story about somebody who they're still suffering three years in, and they're still, you know, that's a horrible thing to hear for somebody who's even, you know, at the beginning of it, you know, it's just unbearable. Yeah? Because
Jules
when you're out, you can look back when I had difficulties for longer than most, yeah, yeah. And I look back and I'm okay, so I can talk about it. But when you're in, it time, as you say, is stretched. So the idea of that for, you know, a year, two years, yeah, you it's like, it's feels unbearable when you've gone through it. Then you can look back and say, I did that, and I could go through it, but at the time, a stretch like that feels,
Julie
yeah, incomprehensible, yeah, that you gotta walk that long with that kind of burden. It just you don't even know how to deal with it. I think, yeah,
Jules Evans
yeah. In journeys like that, you kind of don't want to know the length you just like, because it is unpredictable as well. And I could, we, can, we can eventually maybe help to reduce the length of time that people go through, right? I guess people, you know, sometimes people are looking for explanations. What's going on, what's, what's my theory about what's going on and therefore how I can recover. Did, did you both have that, like, you know, like, searching for a theory is this, oh, yeah, immune system is this neurological? Is this spiritual? You know, yeah, and that's you don't really know. You don't really know
Julie
for sure. Well, and that's where you know sometimes when you're going to these healers or spiritual people, you know, I went back to a shaman who worked with Ayahuasca too. I mean, I was just willing to search anywhere and with anyone, but it's there's a lot of pressure around that you need to sort through the spiritual journey. And so when it's not resolving, I think you keep feeling like somehow I'm not getting it right, and it was interesting. You wrote the article about the extraction, you know, IFS…
Jules Evans
and the entities
Julie
with the entities you don't want to ever have anything to do with not me, either, not me. It wasn't helpful and and anytime somebody talked about that, I went to a women's group, integration group, and they would bring that up, that maybe there's something to that, that's something, you know, connected to my energy or whatever. I hated that. Yeah, that that was not helpful to me. Yeah.
Jules Evans
So, okay, so, how did things start to improve?
Julie
How honestly I had the Depression had gotten so bad. So I finally, I tried a few SSRIs, and I couldn't tolerate them, but I did well at first, like my sleep returned, and so I was really good. I never took anything long term for sleep, and so it but I just, I did not want to get dependent on something for sleep. And so there are some ups and downs, but she suffered with sleep my quality, yeah, but when my quality of sleep returned, that was a blessing. And then I took a lot of cold showers to cold showers were really grounding for me, but I took cold showers before, but sometimes
Jeff
three times a night, yeah, wow, yeah, every few hours
Jules Evans
I'm I'm always interested in how long so kind of different symptoms, because, you know, people have like, 10 or so or more different symptoms, and then some would will stop at different times, and that kind of gradually makes things easier. So when the sleep issues, which was like disturbed sleep, fear of going to sleep, yeah, maybe nightmares.
Julie
So No, no nightmares, but the fear of going to sleep, that or being able to and that was intermixed with then trying these medications. And once I just got off all the medications, and then I was just taking Gabapentin to help with the anxiety, and very small dose of Ativan, then I. I was able to not go up on that because, again, I was so hyper vigilant on not wanting to be dependent, but just managing the day to day anxiety. But between the cold showers and just, I would say, within three months, my sleep started to regulate. My my weight stabilized. I actually, it took that. Took about four months. Don't you think,
Jeff
Oh, it was longer than that. You were going through all this stuff. You were still six.
Julie
No, no, no, I'm talking about my weight stabilized.
Jeff
Oh, your weight, yeah, that, you know,
Julie
like three to four months? I was able to not go up on that because, again, I was so hyper vigilant on not wanting to be dependent, but just managing the day to day anxiety. But between the cold showers and just, I would say, within three months, my sleep started to regulate. My my weight stabilized. I actually, it took that. Took about four months. Don't you think, Oh, it was longer than that. You were going through all this stuff. You were still six. No, no, no, I'm talking about my weight stabilized. Oh, your weight, yeah, that, you know, like three to four months? Yeah, I was, I was feeding her high protein shakes for a while when she first got back, because I was so paranoid about that, and she she did that, and gained a little bit of weight, and then finally, she couldn't do any more of that, my app well, and I had to, because I eat it again appetite. So then my appetite came back. And that was within like six months, you know, I started having a normal appetite.
And, like, by spring, I started doing more social things, so going out hikes with friends and, you know,
and then in, let's see, I think it was July. I started some Lexapro, and just 10 milligrams. And so 10 is the low dose they start you on, and I've never had to go up from that. And so that helped me with my depression and and I stopped crying. Yeah, so that's Yeah, exactly not the morning anxiety she's still having. Yeah, and I had read a few other accounts of people finding that Lexapro was helpful, so we decided to go for that.
Jeff
But she had a really hard time doing it, because there's this whole idea that using any kind of medication is something, well, anti-psychedelic,
Julie
yeah, yeah, yeah, so from that camp, yeah, that the goal was to get off anything. And in fact, the the one gal who I told you, I called and had the consult who had written that article about having her own Ayahuasca trauma. The counselor, when I told her what I was doing, she was like, oh, all those chemicals, you know? And it was just again, right? And that's where my counsellor was so wonderful. She just like, Julie, I'm You're so brave to continue to try all these options and so. But it said the morning anxiety. And so then we just decided to try, well, Bucha, and started with 150
time release. And that was too much. And so I went down to just 100
And I take, so I take that and the Lexapro, and that's it. I mean, occasionally I'll take a 100 GABA, which, you know, the usual dose for that was 303 times a day. So like, if I wake up in the middle of night and I struggle go back to sleep, I'll take 100 of the GABA. But, you know, that is like, and I am just, I'm managing. I mean, and the thing is, is that it's not that I don't have anxiety, but it's situational. It's much more situational. And it's also having, you know, developed a discomfort with anxiety because of what I went through. So there's a part of me that's like, you know, anxiety, you know, isn't good, and so I'm having to befriend certain things again, like, you know, anxiety is a normal part of living in life, and I think there's that little bit of fear, like, I never want to go back to that. So the fear of, you know, I now since so I stopped going to counseling in August, and I haven't used Ativan in over two months. And yeah, I, I quit the job I had. I'm starting a new job, just lots of bought kayaks and paddle boards. And yeah, we're, we're just back to live in our life. Mm, hmm.
Jules
So you are managing to enjoy some aspects of life again.
Julie
Yes, absolutely, yeah.
Jules:
What advice would you give if someone's watching this and at some stage in, in, in in the in that journey. Or, I don't know what metaphor we could use, but let's just say that someone's watching this at some stage of post psychedelic difficulties. What would you say to them?
Julie
They're not alone. Because I think anytime like Deborah Martin was so powerful and you connected me to Deborah, that book, you know, that we ordered and read. When I read that first chapter, I felt like I could have written it
Jules:
this is breaking open.
Julie
Yes, yeah.
Jules:
Thank you for the plug. Okay, well, so this was a collection of 14 people telling their stories of in her case, yes, MDMA triggered extended ego dissolution, and it's a beautiful chapter, isn't it? Oh,
you contacted Deborah
Julie:
we're still in touch. She is just so beautiful. And I had a student who went through it this summer. She did mushrooms and acid end up in the same place, and didn't know where she could go. And the counselor working with her knew I'd been through it, so she came to me, and I also connected her to Deborah, and I connected her to your information as well, but that was the most important thing. Like, you're not alone.
Don't let people pressure you. I had a lot of pressure to do it again, and I felt a lot right, yeah, so the the healers and the people that are in that realm, like, you just gotta go back in. You have to face your fear. You have to do it again. Yeah, that's the answer is to do more and somehow break, break through some, you know, they don't give any space for the fact that it, you know, it could just be traumatic in and of itself. And you're, you know, biochemically, that your body is just Yeah, and, you know, even though I had a great experience with the MDMA, the reality is, anything could, you know, in in Deborah was really I asked her about it too, because she had the experience of MDMA. And she said, Julie, I just, I would make sure your feet are on the ground for a long time before you consider that.
And so you're not alone. These you are going to get better. The hard thing is the unpredictability of it and
to, like, the reconsidering, you know, why you're doing what you're doing, because when I was at the worst for me, like, Why do I continue to get up and face these hardships? I had reasons why, right? That's the values and the commitment I had, these values that I was committed to that helped get me through those moments.
Jules:
And what were they? What was your reason? What were your reasons?
Julie:
My family, so my kids, my grandkids, my husband, you know, he was, he was in it with me like every step of the way one day I said, I said, Jeff, I already feel dead. And he said, Well, then I'm dead too, you know? And so, and trying to figure out who it's safe to be vulnerable with, and finding people that you can feel safe with be okay.
So this was the other thing, being told it's okay to step away from things right, that you might lose relationships over this. I had one woman who is a neighbor, and I love her, but she's very much about, you know, having get togethers and doing all these activities, hockey games and whatever. And I finally had to tell her, like, you know, I am still working through this. I don't understand it. And she said to me, you know, I've been through hard stuff too, but I can't let people drag me down. I was like, Okay, I and I didn't take it personally. It was really weird.
I just said, you know, I don't blame you. We have to protect our own peace of mind. But just know, I had another friend who I talked to, and she said I told her I'd had to start taking out of them every day and and she said, every day, you know, so again, there's so many people that won't understand. You have to find one or two people that that you can connect with and they can reassure you that you're okay, that you're going to be okay.
Jules:
any other kind of, maybe books, articles, podcasts, that were helpful in the storm.
Julie:
Your stuff was the most helpful when I was coming up on a year and Jeff reached out to you, and you gave him that article about the follow up with your research and how many people it took a year that it's not abnormal for it to take that long. Now, while I didn't necessarily want to know that early on, it was so reassuring, right?
Point, it was so reassuring and again, to to just recognize your journey is going to be different than other people's journey. And I even said to you, like, I don't even know if I fit with this group. I said, What about the anxiety? And you said, anxiety is one of the primary things, right? And so it's understanding the array of things that could be a part of this, and that's where your information was so helpful, having somebody look for information for you instead of getting on the internet, because that is an airy play. Yes, she also really benefited from a few other accounts of people that have been through. There's another guy that I can't remember his name offhand, but he had done LSD, and it's something about the title of something how I broke my brain, something like that on LSD. And it was the same kind of situation in that story about how he had done LSD and had this horrific, you know, post difficulties and how he went through it. At one point, he was an adult, and I guess he was maybe 18 when he did it, and he had to sleep with his mother. He wrote because he was so horrified initially, and just didn't know how to deal with it. But he came through it and
and in some respects, talked a little bit about neuroplasticity and stoicism, kind of, although he didn't name it that way, but the same kind of stuff that you have written about, and sort of found a way out of it. And that was really encouraging for her. And then there was another account of a gal who did, uh, mushrooms. I can't remember her name either, and she had major difficulties.
Jules
Rachel Peterson, yeah.
Julie
And so any of those accounts, I think, were priceless, yeah, because you want to know that somebody else and you your story, you know, which I shared with Julie, when I first shared that with her, I mean that it's just a lifeline, you know, to know somebody else has been through it, your story and your research, Yep, yeah.
Jules
Well, kind of lack of information, and, and, and, you know, your story as well is going to, is going to help people as well, because, you know, it's, it's, as you say, that they're priceless. And actually, that's something people say in our research is that other people's stories, people who've been through the same thing, because it is hard to understand if you have through it. I've interviewed you know, veterans who fought in two wars and were injured in wars, and they said their their kind of problems after a psychedelic trip, were involved worse suffering. So it's, it is, you know, this is why it is worth researching as well, because these aren't, these are somewhat rare, you know, maybe 5% of people, but there's a depth of suffering, which is, you know, like trying to help people out of it, you know, well.
Julie
And I wonder Jules, like, just since I've been through this in Idaho, I know of seven different people in Idaho that i is a part of, indirectly or directly my network. And so the student who I worked with on campus and her friend went through has been going through a similar thing. My counselor had a couple people with ketamine who have been completely unraveled and yeah, and she said one of those people went to seven different providers, and they don't know what to do, like between mental health and medical providers, so they throw their hands up. So I feel like there's these places where this stuff is, you know, illegal, and that we just don't even really know the percentage of people that are struggling. I think it might be more widespread than we know.
Jules
Wow, and it's, of course, I Well, I the sympathy I feel as well is like the journey to try and find help and all these different providers, and that can cost a lot of money as well. I mean, so much.
Jeff
And I think also there's a danger, like the psychiatric route too. Can, you know, it's it's not for everyone, and people can fall into the system. And, you know, if they don't have support and they don't understand, I mean, they can, you know, for instance, being committed to a mental hospital and so forth, you can fall into the system. And it can that can be a really hard thing to get out of, too. It could be sort of a self reinforcing thing, if you're branded, you know, to have mental illness. And I think some of the accounts is in maybe even in that book. And other books talk about that too,
Jules
of course, and sometimes these problems can be misdiagnosed. I mean, people can get post psychedelic psychosis, but things like you. Hallucination, persistent perception, disorder, or derealization, or these kinds of things can be misdiagnosed because people just really aren't familiar with them as well. I mean, a lot, and it's just, and there's still a mystery, isn't there as well? Like, you know, you you'll never entirely know. I mean this, like, you know, the shock of energy, and then this kind of nervous system dysregulation, the hypersensitivity. I hear similar kinds of stories, very similar sensitivity, somatic or nervous system dysregulation. And we weren't really, well, we don't know at the moment, like, what, are, you know, these sudden bolts of energy or different things. So one has to, kind of, I suppose, accept that there's well that we come through it, we won't fully understand it.
Julie
But, yeah, yeah, yeah, yeah, but yeah, just just hearing the stories connected to the people who understand it, feeling understood, you know, and again, that's that's such a key that you provided for us is connecting us to those people, and we're so grateful. Yeah, well, it is a network. It is a net.
Jules
Finally, Jeff and Julie. Um, my parents, by the way, I called Jeff and Juliet, but that's anyway, Jeff and Julie, um, what? What message would you have for psychedelic culture and this nascent psychedelic industry?
Julie
People need to be informed. People need even though it's a maybe a rare thing, it is a rare thing. I am. One thing I'm glad about is that I understand now. So if people are talking to me as a counselor about even ketamine like that, there is a potential that we don't understand. And so I think we need both in for, you know, both sides, and I understand the enthusiasm marching forward. It's very exciting.
But my counselor said to me, she said, Julie, at some point, she said, I helped her so much. She said, Julie, this is not just integration, and it's not just trauma. There's another piece to this right that we don't understand, and so it's changing the way that she supports people, and even probably if they start exploring these options, you know, just to be informed and to recognize, I know that there was one gal that had really horrible struggles, but was still involved with a group of people that talked About
being sitters or helping people integrate. And again, they were all very enthusiastic. And she had to keep saying, okay, but you know, there, that's not the whole story. It's not necessarily over when it's over, and that's the piece like you just it's we're dabbling in something that we don't completely understand, and we're doing cultural things that we we haven't been raised in those cultures. And if we're going to Peru, we're putting ourselves in the hands of people that do this stuff all of their lives.
Jules
But it's, it's a complete departure, yeah, from Yeah. In fact, in shabibo culture, it's the shaman who mainly takes the Yes. So the kind of group, you know, let's, let's drink five times in a in a week, or something. This is a, this is a relatively recent Western mention of Western, Yeah, crazy, really? I mean that's yeah, this is not, it's packaged as indigenous wisdom practice…
Julie
yeah, we need, we need to be accountable for what we're inviting people to do. We don't understand it. And even for those providers who are on the end of taking it themselves,
just because that works for them. That's that would be like throwing medication at somebody and saying, Well, this works for everybody
Jules
I know and and then if it's not working for them, shaming them that somehow they need to work through that, that it's not the medicine, that it's them. It wrong. They're harming the need to surrender more. Yeah, right. Well, you, you provided some really amazing advice. Thank you for sharing your experience. Everything mentioned, I'm going to put as links in the kind of YouTube video I you know, I don't know if you'd be okay with sharing the details of your integration therapist as well. Like, maybe, yeah, absolutely. I want to contact because it sounds like they did a good job. Yes, absolutely. And again, being in Idaho, to have somebody as a resource, it's a very hard thing to find, so I will definitely reach out to her and ask her, and I'm sure she'll be happy to have that. Yeah, anything else that I haven't asked about that you'd like to
add,
Julie
just No, just our appreciation for you and the resources you connected us to it. It really can take one person to throw you out a lifeline, and that's what it felt like you did and and just the generosity of you and Deborah and these people who've been through it, I feel like they were the most helpful, honestly, but again, they understand at a level. Then a lot of these people that are doing integration, they don't understand. They don't understand it
Jules
well, there is, there is a network of people who've gone through this, and also similar things like meditation, you know adverse events. You know, people who went to adaptation retreat, and then suddenly, for a year, they're dealing with nervous system dysregulation or derealization or just spontaneously as well, like other people in that book, just out of the, you know, bold kinds of things. So, right? Yeah, they're, they're, you know, amazing. You you've contributed to this, to this network with your stories as well. So I really appreciate it, and I honor what you've been through. I had a little bit of a glimpse of this. No one else will ever know quite what it was like, But you two will like that, that intense journey that you went through. So yeah, just well done for your bravery and resilience and endurance.
These difficulties can encompass various experiences that affect social interaction and connection with others:
Feeling alone in a crowded room
One of the most commonly reported social difficulties is a profound sense of social disconnection. Some individuals describe feeling like an outsider, even among fellow psychedelic users/journeyers. This sense of isolation can leave one feeling distant, withdrawn, and unsure how to bridge the gap between oneself and others.
“A feeling of being distant, withdrawn, ’socially outcast’… Even from other Ayahuasca users.”
Study participant report (Evans et al., 2023)
Struggling to communicate and share
Expressing oneself can become difficult post-trip. Individuals might find it hard to find the right words or feel misunderstood by those who have not shared similar experiences. There may also be a fear of judgment or stigma surrounding psychedelic use, leading to reluctance in opening up about one’s journey.
Dealing with social anxiety and feeling hurt
Some individuals may experience heightened social anxiety after psychedelic use. This can manifest as a fear of being judged or misunderstood by others, leading to avoidance of social situations and increased feelings of isolation.
Individuals may also experience hurt or distress due to the behavior of others, particularly during or after psychedelic experiences. This can include feeling mistreated or invalidated by psychedelic guides or peers.
Withdrawing and longing for normalcy
In more severe cases, individuals may withdraw completely from social interaction, feeling untrusting and disengaged from friends and peers. Individuals may also experience difficulties with being socially ‘normal’, where they want to fit in and be ‘normal’ but no longer know how to do that.
“I became withdrawn, untrusting, disengaged from friends. I recall giving away my possessions. Though smart, I dropped out of high school.”
Study participant report (Evans et al., 2023)
Coping strategies
Reconnecting with others and oneself after a psychedelic journey takes time and effort. Seeking support from understanding communities, therapists, or peer support groups can provide a safe space for individuals to process their experiences and connect with others who can relate. Effective coping strategies commonly reported include reading or viewing materials about the condition, receiving therapy or coaching, spending time outdoors and in nature, and seeking support from peers and family.
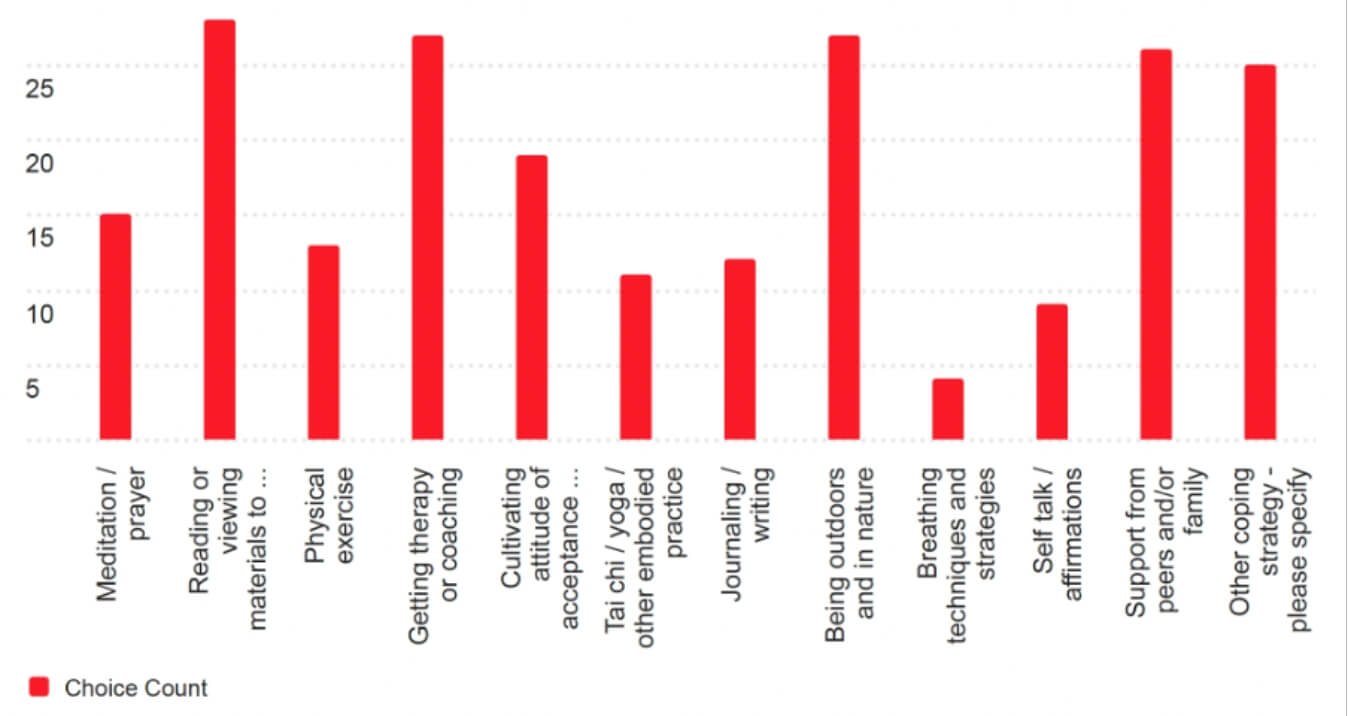
Here are some practices people generally have reported to find helpful to cope with challenging psychedelic experiences:
- Speaking to friends and family or attending a peer support group
- Speaking to a therapist, especially one who is familiar with psychedelics and psychedelic difficulties
- Cognitive practices like compassionate self-talk, cognitive distancing, and especially meditation and prayer
- Embodied self-care practices like exercise, yoga, walking in nature or body relaxation
- Finding useful information online and in books (e.g. the work of Stanislav Grof’s or “Breaking Open: Finding a Way Through Spiritual Emergency” by Jules Evans and Tim Read)
- Journaling
- Engage in creative activities like writing, art-making, or music
- Some people find medication helpful. Additionally, although controversial and risky, some may find that a subsequent altered state experience can help resolve their difficulties. However, this method carries obvious risks and should be approached with caution.
It is essential to explore and integrate these strategies in a way that resonates with personal preferences and needs, seeking support from professionals or trusted sources as needed.
More information
Bibliography
Argyri, E., Evans, J., Luke, D., Michael, P., Michelle, K., Rohani-Shukla, C., Suseelan, S., Prideaux, E., McAlpine, R., Murphy-Beiner, A. & Robinson, O. C. (2024). Navigating Groundlessness: An interview study on dealing with ontological shock and existential distress following psychedelic experiences. Available at SSRN.
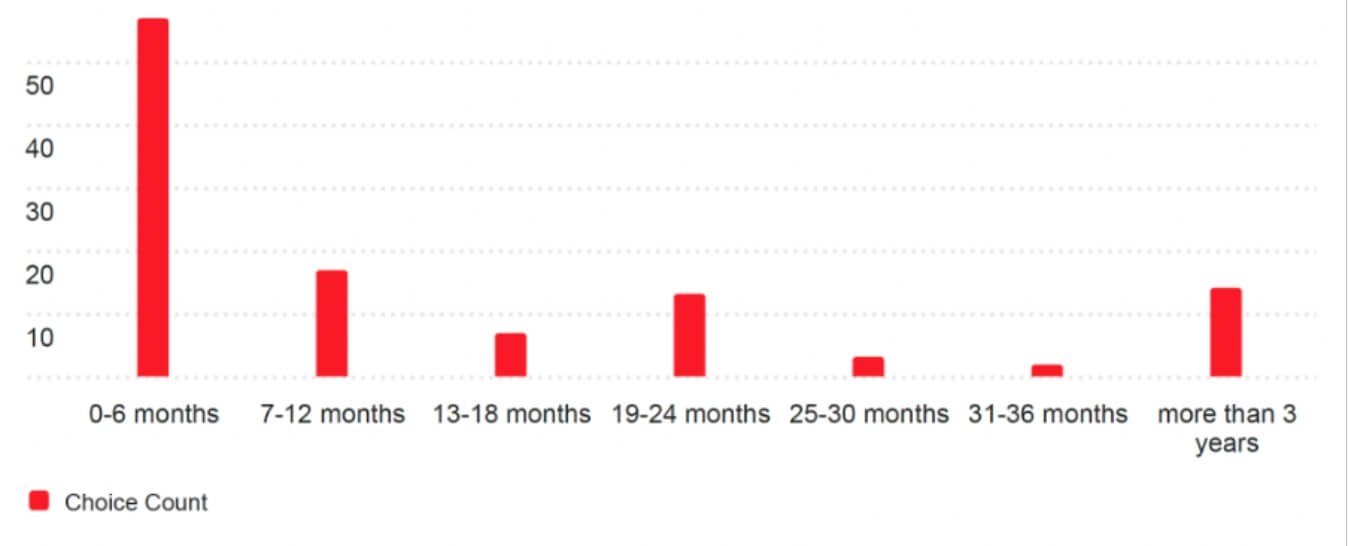
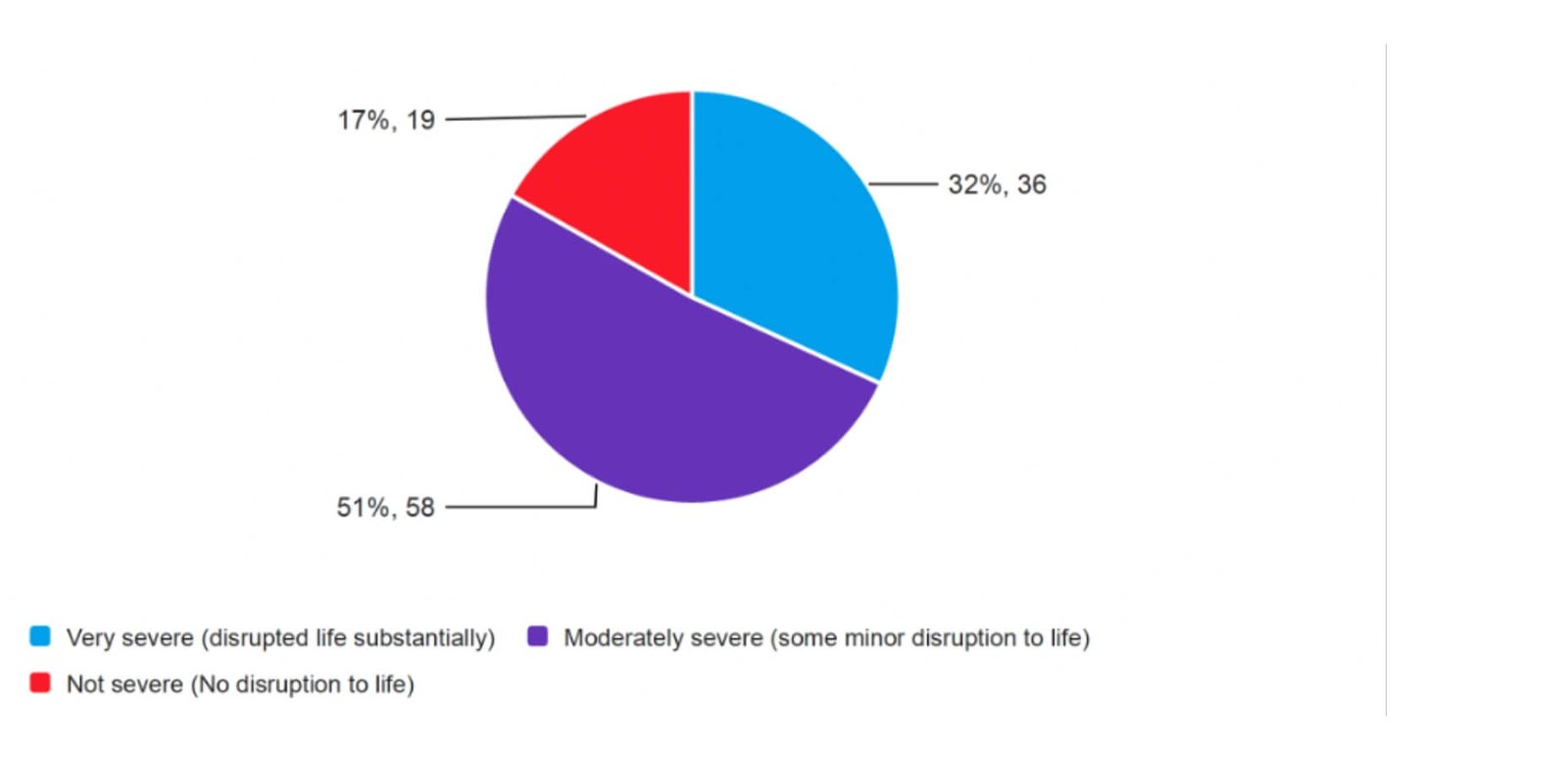
Evans, J., Robinson, O. C., Argyri, E. K., Suseelan, S., Murphy-Beiner, A., McAlpine, R., … & Prideaux, E. (2023). Extended difficulties following the use of psychedelic drugs: A mixed methods study. Plos one, 18(10), e0293349. https://doi.org/10.1371/journal.pone.0293349
Robinson, O., Evans, J., Luke, D., McAlpine, R., Sahely, A., Fisher, A., … & Prideaux, E. (2024). Coming back together: A qualitative survey study of coping and support strategies used by people to cope with extended difficulties after the use of psychedelic drugs. Available at SSRN.